Approximately 50% of patients with C3G progress to kidney failure within 10 years of diagnosis and require dialysis or transplant. C3G may reoccur almost immediately after kidney transplantation and contributes to allograft loss in approximately 50% of patients within 10 years.1-3
Expert biopsy analysis with a renal pathologist is essential to confirmatory diagnosis and evaluating prognosis.2-4
What is Complement 3 Glomerulopathy (C3G)?
C3G is an ultra-rare kidney disease that causes glomerular inflammation5,6
Previously classified within MPGN, C3G was recently reclassified as its own disease state to better acknowledge the causative factors of the disease.7
Unlike CKD, patients with C3G often present as children and young adults, which can place a significant burden on their outlook for the future.8
Hear From a Real Patient Living With C3G9
.
Patient portrayal.
"You can't plan for the future. You don't know where you'll be next year."9
— A real patient with C3G
Patients can be diagnosed with 1 of 2 subtypes of C3G: DDD or C3GN
DDD is usually associated with pediatric cases and may progress more quickly than C3GN.3
C3G can be heterogeneous in clinical presentation and prognosis3,5,6,10

Patients may present with low to heavy levels of proteinuria and hematuria
C3G can be acute, recurrent, or rapidly progressive
Unresolved proteinuria and hematuria may be important indicators of C3G and should trigger expert biopsy analysis.3
A Multidisciplinary Approach Is Key to Help Accelerate the Differential Diagnosis of C3G vs Other Similarly Presenting Glomerulonephritis3
Collaborating with an expert renal pathologist as soon as C3G is suspected can help avoid delayed diagnosis2-4
Accurate, confirmatory diagnosis of C3G requires a multistep process in collaboration with a pathologist, including urinalysis, serology, and biopsy.3
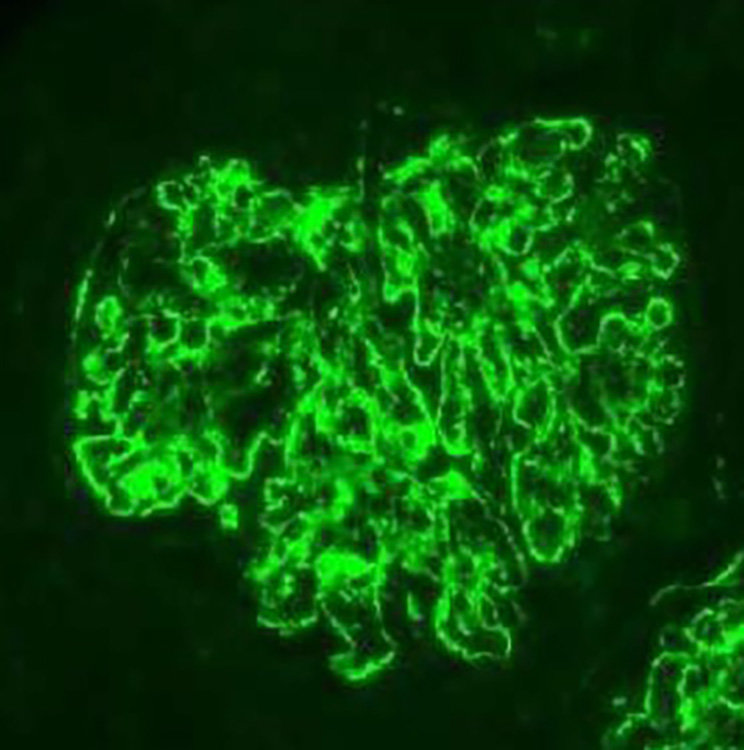
IMMUNOFLUORESCENCE C3-DOMINANT STAINING: AT LEAST 2 ORDERS OF MAGNITUDE GREATER
A biopsy is necessary for a pathologist to evaluate C3 accumulation, as well as glomerular inflammation and injury.1,2,6
Using immunofluorescent analysis of biopsy staining, C3G can be identified by C3 accumulation seen as intense staining at least 2 orders of magnitude greater than any other immune component, with absence or low presence of immunoglobulin and components of the classical complement pathway.2,3
Image credit: Martin B, Smith RJH. C3 Glomerulopathy. 2007 Jul 20 [Updated 2018 Apr 5]. In: Adam MP, Everman DB, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1425/
Once diagnosis is confirmed, the latest ICD-10-CM codes should be used to categorize C3G11
Clinical presentation of C3G can vary among patients, and accurate categorization of C3G diagnosis based on unique manifestation can help inform personalized care.3,11
The latest ICD-10-CM codes recognize C3G and its subtypes with unique coding based on clinical presentation.11 View codes here ↗.
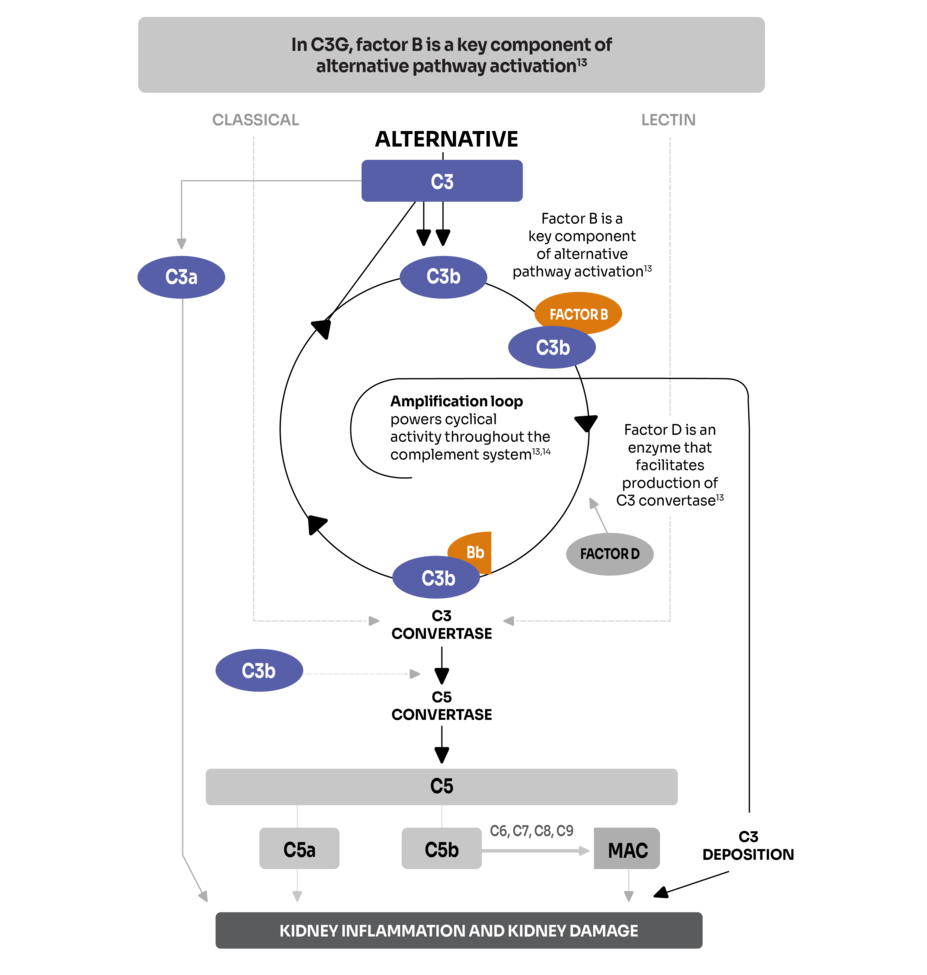
Complement Overactivation Contributes to Disease Progression
In C3G, uncontrolled activation of the alternative complement pathway is the primary driver of disease and kidney damage3,12-14
The alternative pathway is 1 of 3 pathways of the complement system, an innate component of the body's immune system.15
In C3G, uncontrolled activation of the alternative pathway results in the deposition of C3 fragments in the glomerular mesangium and along capillary walls. This disrupts kidney function and causes inflammation.12,14,16
KDIGO guidelines ↗ recommend an in-depth study on the role of the complement system in C3G.17
The Burden of C3G
.
Patient portrayal.
Patients living with C3G are at risk for rapid progression toward kidney failure—some even face the prospect of reaching kidney failure before adulthood3,18-20
Once diagnosed, patients rely on supportive care, steroids, other immunosuppressants, and lifestyle modifications to help slow the rate of progression to kidney failure17-19
Steroids can produce side effects that may need to be managed along with disease symptoms17
Hear From a Real Patient Living With C3G9
.
See the mechanism of disease (MOD) for C3G
View the MOD for C3G
Novartis is committed to addressing unmet needs of people living with complement-mediated kidney diseases.