Heterogeneity in IgA Nephropathy
The heterogeneity of clinical and pathological features, as well as disease progression journey of IgA nephropathy (IgAN), may demand a tailored approach to care1,2
Clinical presentation can vary2,3:
Asymptomatic: microscopic hematuria and/or proteinuria
Symptomatic: gross hematuria, foamy urine, or nonspecific symptoms related to presence of hypertension and kidney decline
Pathological features2,3:
The level of C3 accumulation in the glomeruli can vary among patients and may be an indicator of prognosis
Disease progression2,3:
Progression to kidney failure following biopsy has ranged from ~5 years to ~30 years across ethnic populations
The Heterogenous Nature of IgAN Requires You to Understand Each Patient's Disease1
Patients with IgAN, the most common primary glomerulonephritis, face both physical and emotional burdens. The diverse clinical and pathological features, coupled with potentially unpredictable disease progression, can call for an understanding of each patient's disease based on symptoms.1,4
Patients may present with various clinical signs1
Some patients will still have persistent proteinuria despite optimized supportive care1,*

Some patients may experience signs of glomerular inflammation along with proteinuria, including1,5,6:
- Persistent hematuria OR
- Different rates of eGFR decline OR
- MEST-C scores that may vary depending on severity
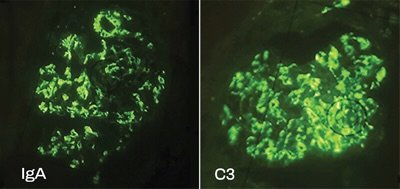
Image showing colocalization of C3 and IgA in a kidney biopsy.
You may see varying amounts of C3 and IgA deposition in your patients’ biopsies7
Image adapted from: Mastrangelo A, Serafinelli J, Giani M, Montini G. Clinical and pathophysiological insights into immunological mediated glomerular diseases in childhood. Front Pediatr. 2020;8:205. doi:10.3389/fped.2020.00205. License: https://creativecommons.org/licenses/by/4.0/
Implications for disease management

A multidisciplinary approach is key to developing a care plan for your patients1
The heterogeneity of IgAN calls for you to understand each patient’s disease1
ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; C3, complement 3; eGFR, estimated glomerular filtration rate; MEST-C, mesangial hypercellularity (M), endocapillary hypercellularity (E), segmental glomerulosclerosis (S), tubular atrophy (T), and crescents (C).
References: 1. Rovin BH, Adler SG, Barratt J, et al. Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100(suppl 4):S1-S276. doi:10.1016/j.kint.2021.05.021 2. Yeo SC, Goh SM, Barratt J. Is immunoglobulin A nephropathy different in different ethnic populations? Nephrology (Carlton). 2019;24(9):885-895. 3. Rajasekaran A, Julian BA, Rizk DV. IgA nephropathy: an interesting autoimmune kidney disease. Am J Med Sci. 2021;361(2):176-194. 4. Feldman DL, White EM, Julian B, et al. The Voice of the Patient: Externally Led Patient-focused Drug Development Meeting on IgA Nephropathy. National Kidney Foundation; 2020:1-87. 5. Pitcher D, Braddon F, Hendry B, et al. Long-term outcomes in IgA nephropathy. Clin J Am Soc Nephrol. 2023;18(6):727-738. doi:10.2215/CJN.0000000000000135 6. El Karoui K, Fervenza FC, De Vriese AS. Treatment of IgA nephropathy: a rapidly evolving field. J Am Soc Nephrol. 2024;35:103-116. doi:10.1681/ASN.0000000000000242 7. Mastrangelo A, Serafinelli J, Giani M, Montini G. Clinical and pathophysiological insights into immunological mediated glomerular diseases in childhood. Front Pediatr. 2020;8:205. doi:10.3389/fped.2020.00205
